What Women Need to Know About Strokes and Heart Attacks

When Andrea, a 35-year-old Nashville, Tennessee, woman called 911 because she thought she was having a heart attack, the emergency medical technicians told her she was likely just experiencing a bout of anxiety.
“They made me walk outside, down my driveway to the ambulance. They never turned on the sirens or lights and stopped at every light on the way to the hospital,” she told Today.
But Andrea was not having an anxiety attack. Instead, it was discovered she had experienced a major cardiac event as a result of a spontaneous coronary artery dissection, an uncommon condition that can affect otherwise healthy individuals.
“The delay in my care caused me to have severe heart damage and heart failure that I am still living with” she said.
While Andrea’s condition is rare, her experience with emergency care is not. When it comes to serious health conditions like heart attack and stroke, women are more likely to be misdiagnosed and receive delayed care.
How Are Symptoms of Heart Attack and Stroke Different for Women?
Myocardial infarction, more commonly known as a heart attack, occurs when the flow of oxygen-rich blood to the heart becomes blocked.
A heart attack can be caused by:
- The full or partial blockage of an artery as a result of plaque buildup.
- A coronary spasm, in which a coronary artery tightens and cuts off blood flow.
When people think of what a heart attack looks like, they might picture a man grabbing his chest and describing severe pain that extends to his arm. While chest pain is the most notable symptom of a heart attack, many people— especially women—experience less common symptoms. This can lead to misdiagnosis and delayed treatment among female patients.
According to a study from the American Heart Association, almost 62% of women who have a heart attack experience more than three non–chest pain symptoms, compared to 54.8% of men.
The perception of which symptoms necessitate emergency care can lead women to delay seeking treatment, which affects their chances of surviving and making a full recovery.
“If you have nausea and vomiting and back pain or epigastric pain … the first thing that comes to you is not, ‘I’m having a heart attack,’” said Melissa Frisvold, PhD, CNM, APRN, faculty at the Georgetown University School of Nursing.
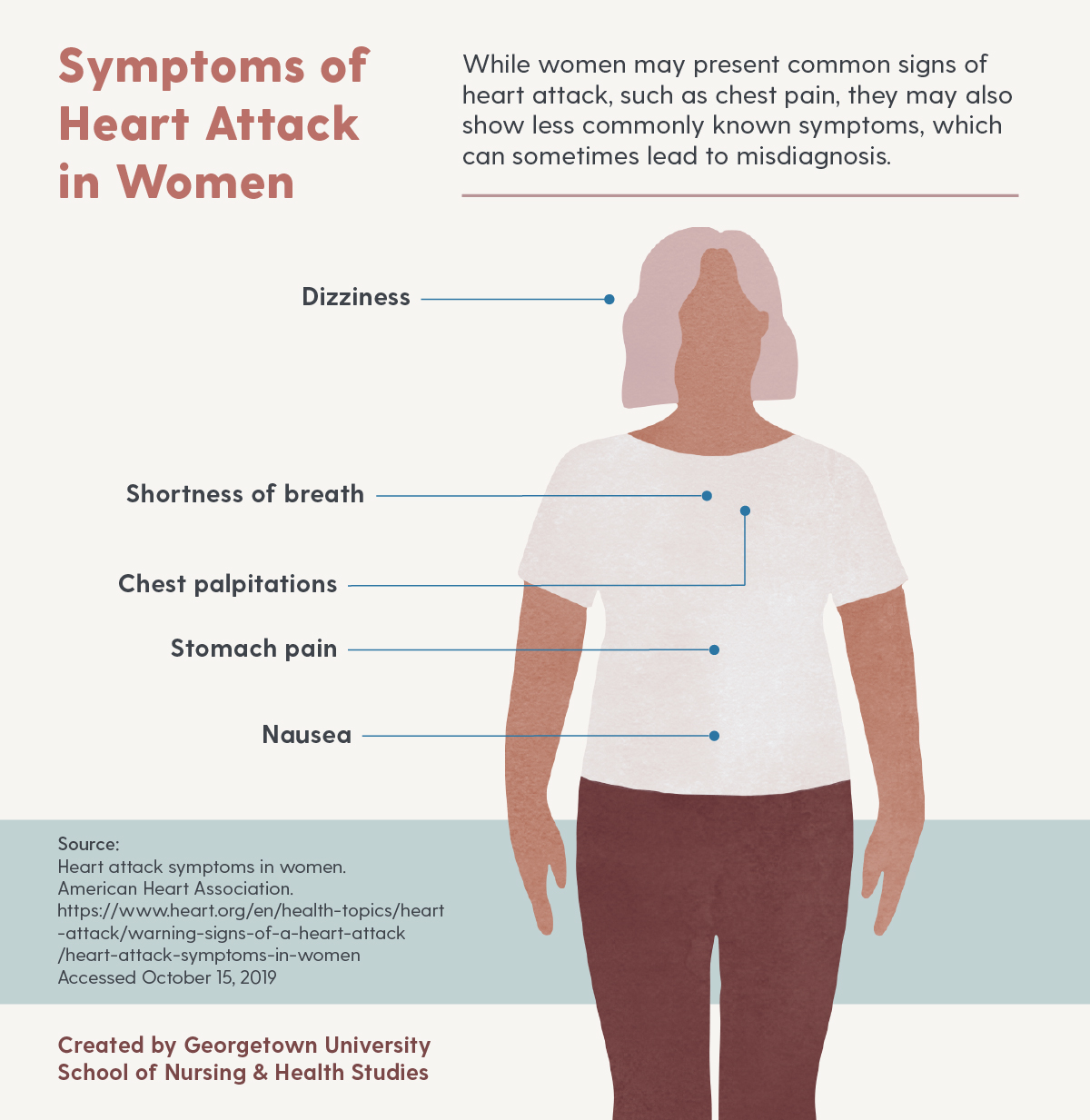
Less commonly known symptoms of heart attack that are more likely to be present in women than men include stomach pain, shortness of breath, chest palpitations, nausea, and dizziness.
For women, perceptions of symptoms can also affect treatment of another life-threatening condition — stroke.
Sometimes referred to as a “brain attack,” a stroke occurs when a clot blocks the blood supply to the brain or when a blood vessel in the brain bursts.
The three main types of stroke include:
- Ischemic stroke — occurs when blood flow through the artery that supplies oxygen-rich blood to the brain becomes blocked.
- Hemorrhagic stroke — caused by a leak or rupture in an artery in the brain.
- Transient ischemic attack — also referred to as a “mini-stroke,” blood flow to the brain is blocked for a short time and is a warning for future stroke
In a 2014 study, researchers found that women experiencing a stroke were at greater risk than men for misdiagnosis in the emergency room. They attributed this disparity to a greater frequency of non-classic stroke presentations, including headache and dizziness.
In addition to having misinformation about symptoms of heart attack and stroke, Frisvold said women may also put more focus on other health risks that they perceive to be bigger threats.
According to the Centers for Disease Control and Prevention’s (CDC) report on the leading causes of death in 2017 (PDF, 2.4 MB), women were most likely to die as a result of heart disease, followed by cancer. Stroke was the fourth-leading cause of death in women.
“Women worry about breast cancer or cervical cancer,” she said. “But heart disease is the leading cause of death in women, not breast cancer or cervical cancer.”
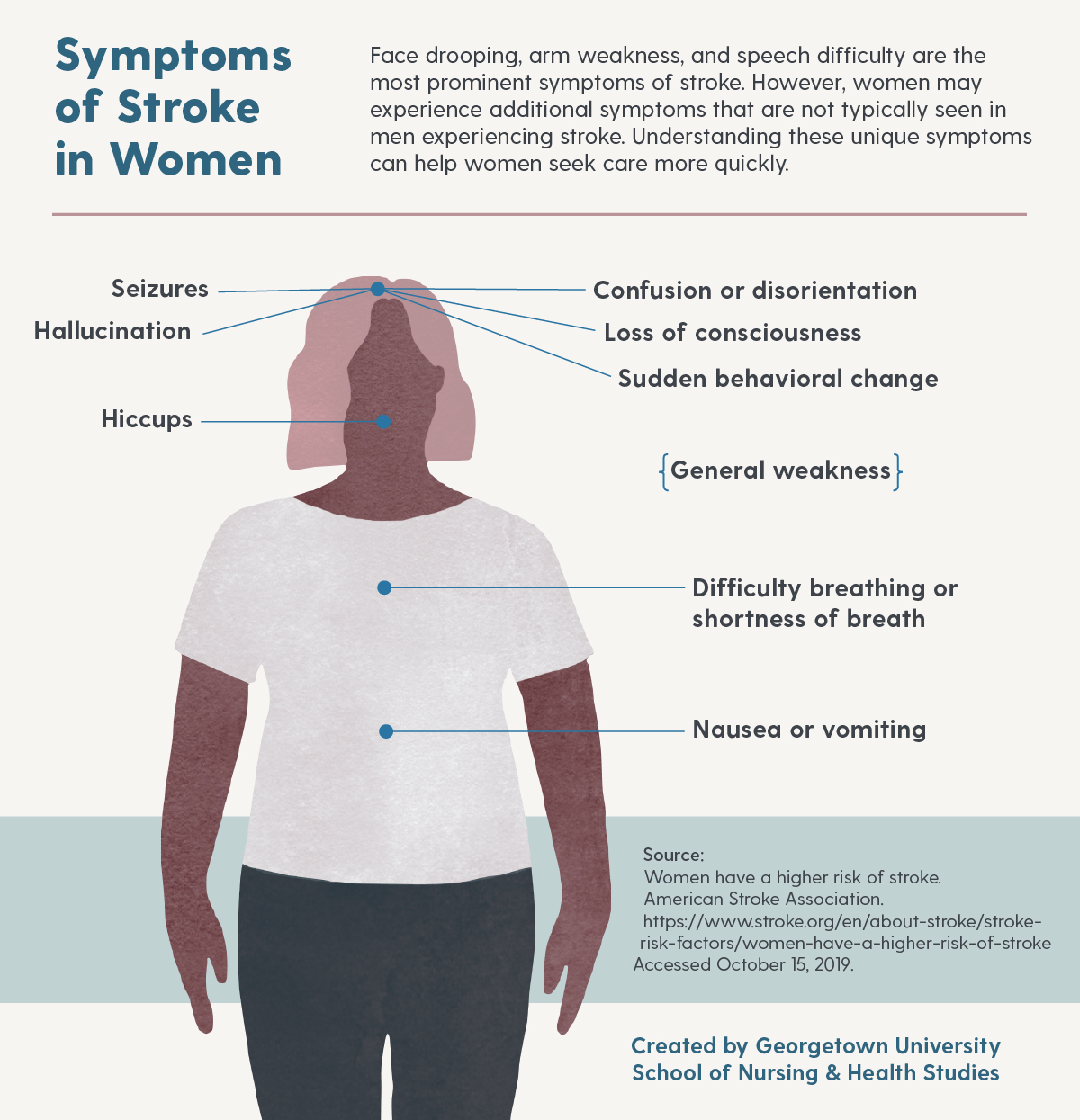
Less commonly known symptoms of stroke that are more likely to be present in women than men include loss of consciousness, general weakness, difficulty breathing, disorientation, sudden behavioral change, hallucination, nausea or vomiting, seizures, and hiccups.
How Does Gender Affect Health Care?
The misdiagnosis of heart attack and stroke in women is part of the larger issue of gender bias in health care. This stems in part from how clinical research has been performed in the past, which informs how care is provided to patients today.
In a research study on sex bias in clinical studies from the Allen Institute for Artificial Intelligence, researchers examined medical research from 1993 to 2018 and found that women were underrepresented subjects in the research of several health conditions, including cardiovascular health.
— Melissa Frisvold, PhD, CNM, APRN
Another study on clinical trials for stroke treatment indicated that women were underrepresented in such trials, leading to suboptimal conclusions for women in outcomes and stroke care delivery.
The exclusion of marginalized groups, including women and people of color, may lead to a misunderstanding of the many ways a health condition can present itself and how it should be treated. “Medical bias,” a term for that disparity, refers to cases in which an individual may receive different care from a provider who is unknowingly acting on partial judgement.
The consequences of implicit bias in health care can be seen in how women receive treatment in comparison to men in life-threatening situations.
For example, a study from the American Stroke Association found that in cases of ischemic stroke, men were more likely than women to receive ultrafast Alteplase administration, a clot-busting drug that helps restore blood flow to the brain.
Additionally, in the aforementioned study from the American Heart Association, 53% of young women (aged 18 to 55) said their health care provider did not think their initial symptoms were heart-related, compared to only 37% of young men who said their provider got it right. These researchers also discovered a pattern in female patients who said they hesitated to seek help because they feared being labeled a hypochondriac.
Because of women’s experiences with the health care system, these biases may affect how women view their own health.
What Can Be Done to Advocate for Women’s Health?
Women, their family members and friends, and even bystanders can take steps to help improve care for heart attack and stroke. From advocating for oneself in the emergency room to taking action when someone is in distress, the following resources are a starting point for women’s health advocacy.
How to Communicate With Your Clinician
Women sometimes express that they do not feel heard by their provider when sharing health concerns. Frisvold provided these tips for self-advocacy.
BRING A FRIEND OR FAMILY MEMBER
Another person can provide support, ask additional questions, and help navigate the treatment process.
BE DIRECT
If an individual believes he or she may be having a heart attack or stroke, being prepared to specifically communicate all concerns to the clinician can help.
ASK QUESTIONS
Engaging in dialogue allows for an individual to push back in a way that is specific and may help a provider check his or her bias.
DON’T LET SELF-BIAS GET IN THE WAY
“When you talk to somebody who had a heart attack, they [often] say, ‘I just knew something wasn’t right, but I just kept trying to downplay it.’ You’re better off going to the emergency room and finding out it was nothing than to err the other way,” Frisvold said.

How Bystanders Can Take Action in Health Emergencies
When another person appears to be experiencing a heart attack or stroke, there are steps that can be taken to help improve the chances of a positive health outcome.
DON’T HESITATE TO CALL 911
“Time is of the essence,” Frisvold said. “Those early moments are critical. Steps can be taken early in the process to improve the health outcome of the person experiencing a heart attack or stroke.”
ASK QUESTIONS
If a stroke is suspected and the person is conscious, the bystander should ask what symptoms the individual is experiencing so the information can be shared with emergency responders if the situation worsens and requires an advocate.
GIVE CPR IF NEEDED
A 2019 study showed that women were less likely to receive CPR from a bystander than men. This step is critical in cases where an individual goes into cardiac arrest while waiting for emergency response. If the bystander is not trained in CPR, a 911 dispatcher can provide guidance in performing chest compressions.
Resources for Further Reading
- Office on Women’s Health — Heart Disease and Stroke
- American Heart Association — Heart Attack Symptoms in Women
- Centers for Disease Control and Prevention — Women and Heart Disease
- National Heart, Lung, and Blood Institute — Heart Attack Information
- American Stroke Association — Women Have a Higher Risk of Stroke
- Centers for Disease Control and Prevention — Women and Stroke
- National Institute of Neurological Disorders and Stroke — Stroke Information
Citation for this content: Nursing@Georgetown, the online MSN program from the School of Nursing & Health Studies


