Maternal Health Around the World
Maternal deaths are primarily attributed to a lack of accessible, affordable prenatal and perinatal care and to unattended births in regions where certified medical professionals are limited. However, maternal deaths are still prominent in countries with advanced systems of health care.
The United States spends more money on hospitalization for pregnancy and childbirth than every other country in the world. Yet, the rate at which mothers are dying as a result of pregnancy or childbirth in the United States continues to rise.
The World Health Organization (WHO) estimated 14 maternal deaths per 100,000 live births in the United States in 2015 (PDF, 1.5 MB); other studies suggest the rate of maternal deaths in the United States is much higher, with estimates up to 28 deaths per 100,000 live births, according to an analysis for the 2015 Global Burden of Disease Study from the Institute for Health Metrics and Evaluation (PDF, 12.9 MB).
To address the issue, the United Nations Millennium Development Goals mobilized medical care providers, volunteers, researchers, and policymakers to work toward universal access to maternal health care from 1990 to 2015; the global efforts toward improving maternal health are now extended through 2030.
Nursing@Georgetown created this resource to explore how the U.N. goals have affected maternal death rates and how these deaths can be mitigated — both in the United States and globally.
Maternal Health: U.S. Versus the World
2030 marks the target date of the United Nations Sustainable Development Goals — a set of benchmarks agreed upon by all countries and leading development institutions — to deliver better health care outcomes globally. One goal is to improve maternal health and access to care, which can be measured by a decline in maternal deaths.1
The Goal
Reduce maternal deaths by
2/3 worldwide.2
The Problem
Every year an estimated 303,000 women
die during pregnancy, childbirth, or soon after.3
This is 830 women every day or
1 woman every 2 minutes.3
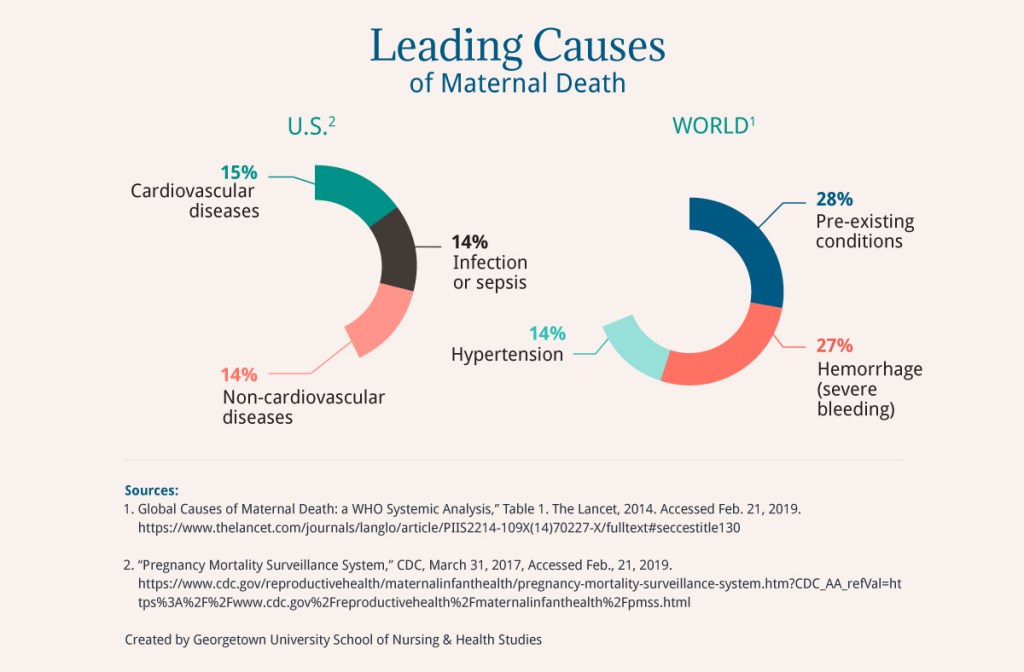
Leading causes of maternal death vary between the United States and the rest of the world. Globally, the leading causes of maternal deaths are pre-existing conditions. In the United States, the leading cause is cardiovascular disease.
Go to a tabular version of “Leading Causes of Maternal Death.”
Maternal Mortality in U.S and the World
The World Health Organization quantifies maternal deaths using the maternal mortality ratio, or MMR, which represents the number of women who die for every 100,000 live births. A lower MMR is better than a higher MMR.
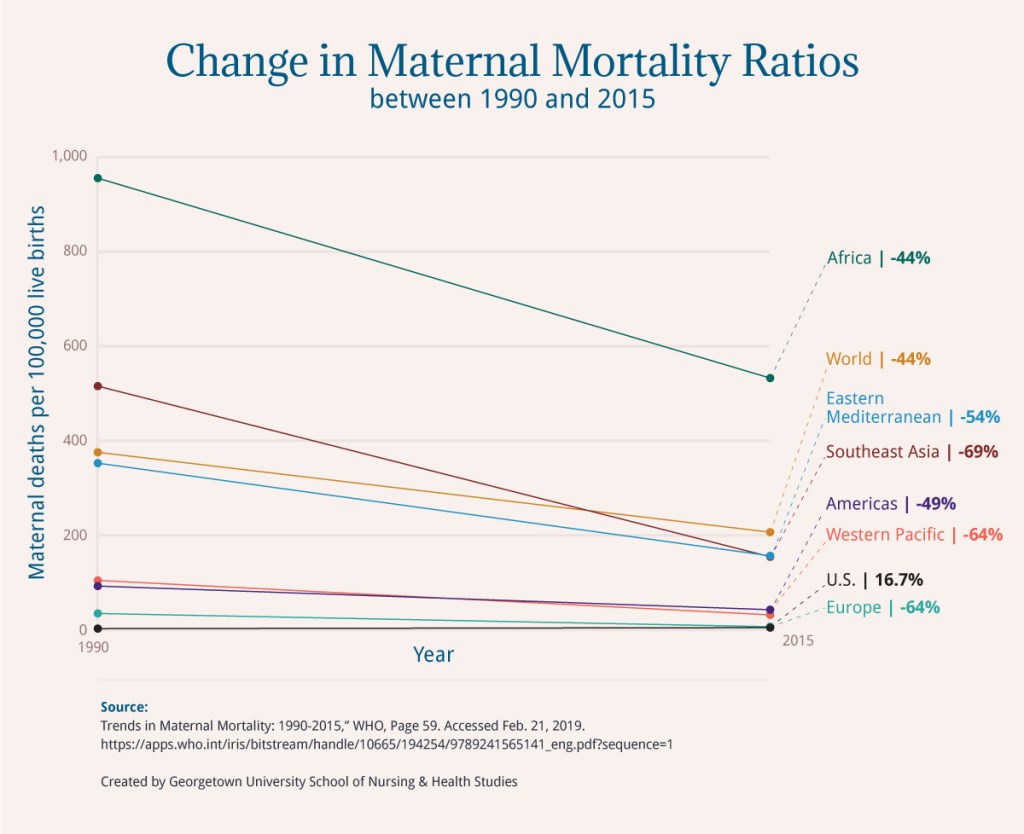
Based on data from the World Health Organization, it is clear that while the world is making strides in reducing maternal deaths, the United States is falling behind. Globally, maternal deaths decreased 44 percent from 1990 to 2015 while in the United States they increased almost 17 percent.
Go to a tabular version of “Change in Maternal Mortality Ratios between 1990 and 2015”.
Behind the MMR Numbers
1 in 180
The global adult lifetime risk of maternal mortality (i.e., the probability that a 15-year-old woman will die eventually from a maternal cause).4
$111 billion
The amount the U.S. spends each year on hospitalization for pregnancy and childbirth — the highest in the world.5
0
Federal requirements in the U.S. to report maternal deaths.6
31.9%
The cesarean section rate in the U.S. in 2016.7 The WHO has stated that rates should stay between 5 percent and 15 percent.8 The risk of maternal death associated with planned cesarean delivery is higher than those associated with planned vaginal delivery.9
The Midwifery Model
Since 1990, the 21 countries that have been most successful in reducing maternal deaths substantially increased facility birthing, and many have done this through the deployment of midwives.10
Studies in both the United States and other countries have documented the positive outcomes of the midwifery model of care. In one such study, researchers found that 45 percent of the women with uncomplicated pregnancies were better off under the care of midwives than in a hospital during birth.11
Goals for the Future
The 2015 worldwide goal for reducing maternal deaths by 75 percent was not met. However, the progress made indicates that a global MMR of less than 70 is achievable by 2030.12
The United States has set a goal of achieving an MMR of 11.4 by 2020.13
To learn more, and to find out information on how you can help in your country or community, visit WHO.int and AmnestyUSA.org.
The following section contains tabular data from the graphics in this post.
Leading Causes of Maternal Death
| World | U.S. |
|---|---|
28% Pre-existing conditions | 15% Cardiovascular diseases |
27% Hemorrhage (severe bleeding) | 14% Non-cardiovascular diseases |
14% Hypertension | 14% Infection or sepsis |
Back to Leading Causes of Maternal Death graphic.
Change in Maternal Mortality Ratios between 1990 and 2015
| Location | 1990 | 2015 | Percent Change |
|---|---|---|---|
U.S. | 12 | 14 | 16.7 |
Africa | 965 | 542 | -44 |
Americas | 102 | 52 | -49 |
Eastern Mediterranean | 362 | 166 | -54 |
Europe | 44 | 16 | -64 |
South-East Asia | 525 | 164 | -69 |
Western Pacific | 114 | 41 | -64 |
World | 385 | 216 | -44 |
Back to Change in Maternal Mortality Ratios graphic.
Sources
1 “The Sustainable Development Goals Report 2016,” United Nations. Accessed Feb. 21, 2019. https://unstats.un.org/sdgs/report/2016/ arrow_upward
2 “Good Health and Well-being.” The Sustainable Development Goals Report 2016. United Nations. Accessed Feb. 21, 2019. https://unstats.un.org/sdgs/report/2016/goal-03/e arrow_upward
3 “Maternal Mortality,” WHO, Feb. 16, 2018. Accessed Feb 21, 2019. https://www.who.int/en/news-room/fact-sheets/detail/maternal-mortality arrow_upward
4 Trends in Maternal Mortality: 1990-2015,” Page 20. Accessed Feb. 21, 2019. https://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf?sequence=1 arrow_upward
5 Kasthurirathne, S. N., Mamlin, B. W., Purkayastha, S., & Cullen, T. “Overcoming the Maternal Care Crisis: How Can Lessons Learnt in Global Health Informatics Address US Maternal Health Outcomes?” AMIA Symposium, 2017. Accessed Feb. 21, 2019. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5977676/ arrow_upward
6 “Pregnancy Mortality Surveillance System,” CDC, March 31, 2017, Accessed Feb. 21, 2019. http://www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html.arrow_upward
7 “Births: Method of Delivery.” CDC, March 31, 2017. Accessed Feb. 21, 2019. https://www.cdc.gov/nchs/fastats/delivery.htm arrow_upward
8 “The Global Numbers and Costs of Additionally Needed and Unnecessary Caesarean Sections Performed per Year: Overuse as a Barrier to Universal Coverage,” WHO, 2010, Page 5, Accessed Feb. 21, 2019. http://www.who.int/healthsystems/topics/financing/healthreport/30C-sectioncosts.pdf arrow_upward
9 “Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term,” CMAJ, Feb. 13, 2007, Accessed Feb. 21, 2019. http://www.cmaj.ca/content/176/4/455.short. arrow_upward
10 “Midwifery: An Executive Summary for the Lancet’s Series,” The Lancet, June 2014, Page 2, Accessed Feb. 21, 2019, http://www.thelancet.com/pb/assets/raw/Lancet/stories/series/midwifery/midwifery_exec_summ.pdf. arrow_upward
11 “British Regulator Urges Home Births Over Hospitals for Uncomplicated Pregnancies,” New York Times, Dec. 3, 2014, Accessed Feb. 21, 2019. http://www.nytimes.com/2014/12/04/world/british-regulator-urges-home-births-over-hospitals-for-uncomplicated-pregnancies.html arrow_upward
12 “Trends in Maternal Mortality: 1990-2015,” WHO, Page 1, Accessed Feb. 21, 2019, https://apps.who.int/iris/bitstream/handle/10665/112682/9789241507226_eng.pdf;jsessionid=E59CC6792B989F6DDAEF73FDC34BEE99?sequence=2 arrow_upward
13 Maternal, Infant, and Child Health.” U.S. Department of Health and Human Services. Accessed Feb. 21, 2019. https://www.healthypeople.gov/node/3492/data-details arrow_upward


