How Will the Nurse Shortage Affect Your State?
As health care evolves in the United States, nurses play a critical role in meeting a growing demand. The aging baby boomer population and the implementation of the Affordable Care Act contribute to the predicted need for health care professionals — especially in primary care. With their training and skills, nurse practitioners (NPs) can help alleviate the projected shortage of primary care providers.
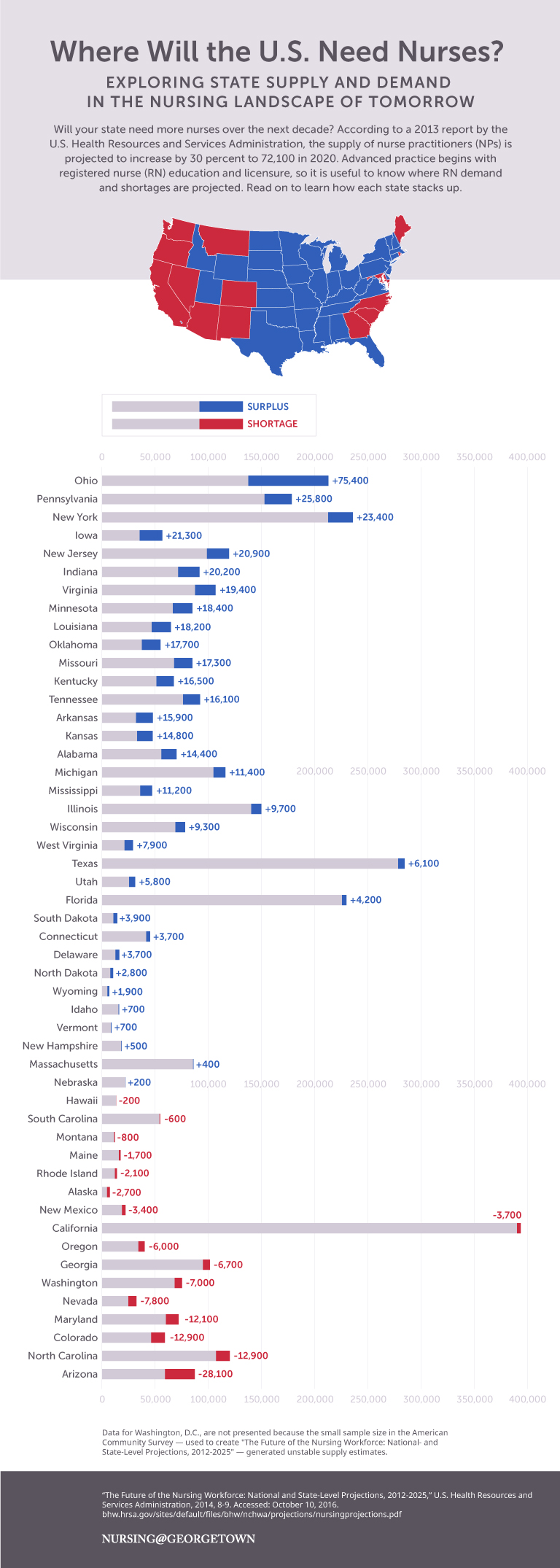
The supply of NPs is projected to increase by 30 percent to 72,100 by 2020, according to a 2013 report by the U.S. Health Resources and Services Administration (HRSA). Advanced practice nursing begins with registered nurse (RN) education and licensure, so it is useful to know the RN demand and projected shortages.
Nursing@Georgetown created the graphic below — based on data from a 2014 HRSA report, “The Future of the Nursing Workforce: National- and State-Level Projections, 2012-2025” — to help illustrate which states will need more nurses over the next decade.
Understanding the Nurse Workforce
The American Association of Colleges of Nursing notes that an aging population, coupled with “nursing schools across the country … struggling to expand capacity to meet the rising demand for care given the national move toward health care reform,” will result in a shortage of nurses.
A 2015 report produced by the Georgetown University Center on Education and the Workforce — “Nursing: Supply and Demand Through 2020” — factors in the age and makeup of the current nurse workforce, the size of graduating nursing classes, and nurses’ career decisions to predict a dearth of approximately 193,000 professional nurses in the United States by 2020. A 2012 report, “United States Registered Nurse Workforce Report Card and Shortage Forecast,” concurs. It predicts a nursing shortage by 2030 throughout the country, especially in the West and South, because of projected changes in population.
The Pursuit of Nursing
Predictions vary regarding the degree of the nurse scarcity ahead, but some regions, like Southern states, have a higher predicted need for health care professionals. Aging population growth and policy changes enable more individuals to access health care, but an inadequate nurse supply can have a significant impact on the availability of quality care, thereby increasing negative patient outcomes.
State-specific scope of practice regulations for NPs will also affect health care. In states that support full practice for NPs, advanced practice nurses can function as primary care providers, which can help to alleviate the anticipated dearth of primary care physicians. However, states with restricted practice regulations, such as California and Texas, cannot take full advantage of care NPs provide. In states with both a predicted nurse shortage and restricted NP practice, shortfalls in RNs and NPs will likely have greater impact on patient care. This will affect many Southern states, including Georgia and South Carolina.
The projected nursing shortfall has a patchwork of causes. Some experts find that the main element is the fluctuating number of students pursuing nursing studies. Other factors include a demanding job environment; inconsistent wages; and challenges to recruitment, training, and retention. Rural areas are more vulnerable to such factors, especially in the Western and Southwestern regions of the United States.
As the authors of “Nursing: Supply and Demand through 2020” explain, “Stressful working environments, along with long hours and erratic schedules in some nursing positions, contribute to many nurses moving in and out of the field based on economic conditions and personal circumstances.” According to the report, of the 5.2 million licensed nursing professionals in 2013, only 3.6 million worked as a nurse during that time.
The report also found that many of today’s nursing schools are not equipped to meet the needs of students interested in pursuing the nursing profession. In the 2011-2012 school year, Bachelor of Science in Nursing programs rejected 37 percent of qualified applicants; associate degree programs rejected 51 percent of qualified applicants. These programs are limited by lack of adequate faculty and facilities to meet educational needs.
Conclusion
Registered nurses can advance their careers to help meet growing demand in the years ahead. Programs like Nursing@Georgetown’s Master of Science degree in Nursing online offer an opportunity for nurses to continue to practice their profession, simultaneously advancing their careers and fulfilling future needs in their communities.
Please note that this blog post is for informational purposes only. Individuals should consult their health care professionals before following any of the information provided. Nursing@Georgetown does not endorse any organizations or websites contained in this post.


