Supporting Women Recovering From Trauma and PTSD

A few days after a difficult labor and debilitating birthing experience, Amanda began showing symptoms of post-traumatic stress disorder (PTSD). In Solace for Mothers, an online community for mothers who have experienced birth trauma and, often, post-traumatic stress disorder, Amanda said she had the strange sensation that she was sitting in a room by herself watching everything else on a television screen.
“It was like my surroundings were separated from me by a sheet of glass,” she wrote.
Women share their symptoms and stories in forums like Solace for Mothers, connecting with others across the country with similar experiences. Through each other, they find support and understanding that sometimes is lacking from their own networks of family and friends. Even clinicians may struggle to fully understand how PTSD specifically affects women.
“I’ve seen how prevalent mental health issues are in the primary care arena,” said Georgetown University School of Nursing & Health Studies faculty member Sally Huey, DNP, APRN, FNP-BC. “Oftentimes, providers are not equipped or don’t have the confidence level to deal with these types of concerns.”
PTSD is commonly associated with men who have survived combat. But women are twice as likely as men to develop PTSD, according to the American Psychological Association. Between 10% and 12% of women will develop PTSD in their lifetime compared to 5% to 6% of men.
With so many women affected by PTSD, what do loved ones and care providers need to know?
What Is PTSD?
The American Nurses Foundation’s PTSD Toolkit for Nurses defines PTSD as a mental health condition that develops as a reaction to and re-experiencing of a traumatic event. Symptoms of PTSD can include nightmares, flashbacks, intense anxiety, and uncontrollable thoughts about the trauma. A study published in Archives of Psychiatric Nursing further notes that PTSD is associated with poor mental health outcomes including negative problem solving, isolation, depression, anxiety, and somatization — the outward, physical signs of inward, psychological concerns.
What Is the Difference Between Complex PTSD and Simple PTSD?
Post-traumatic stress disorder is the official classification in the Diagnostic and Statistical Manual of Mental Disorders that clinicians use to diagnose patients. PTSD is a broad category that describes the wider range of symptoms experienced by trauma survivors, including avoidance, intrusion, and nervous arousal.
This original diagnosis was built on the symptoms of military trauma and the notion of PTSD caused by a concrete, traumatic event — such as experiencing an earthquake, witnessing a school shooting, or watching the violent death of a friend. The kind of PTSD that can develop after such events is now called “simple PTSD.”
Complex trauma, on the other hand, is exposure to traumatic circumstances — not one single event, but repeated experiences that destroy one’s sense of safety in the world. These experiences are often interpersonal in nature and begin in childhood. People who endure complex trauma are more likely to develop complex PTSD (c-PTSD) and demonstrate symptoms different from simple PTSD.
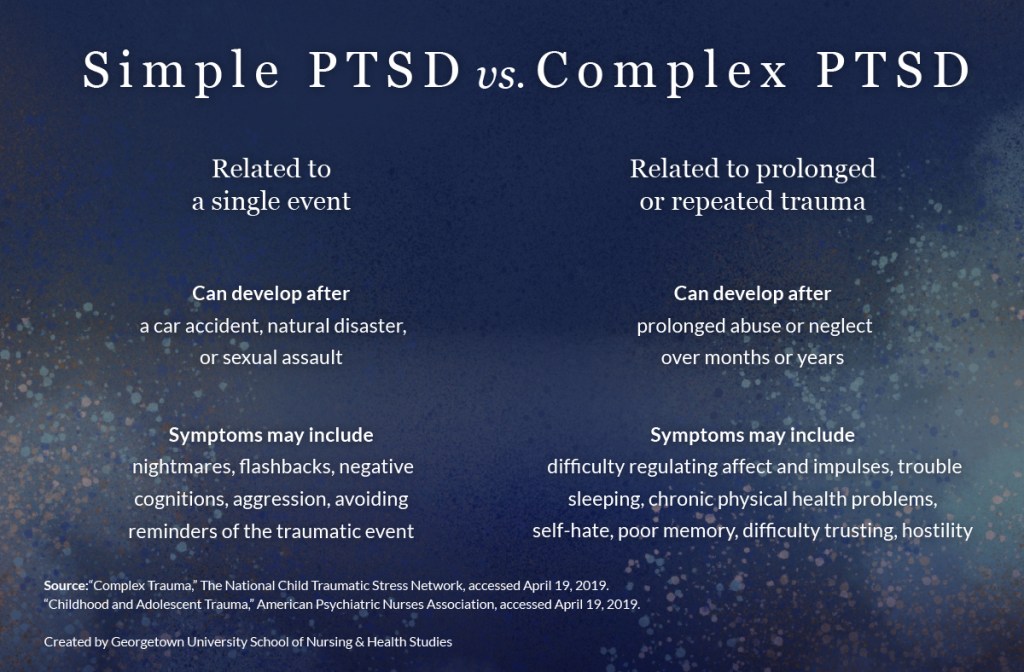
Complex PTSD differs from simple PTSD in that it occurs as a result of prolonged trauma instead of a single event. Behavioral and physical symptoms are more common with complex PTSD whereas simple PTSD symptoms are more psychological in nature.
Why Are Women More Likely to Develop PTSD, Particularly c-PTSD?
PTSD is an anxiety disorder that develops as a protective mechanism to keep an individual from future harm. The nervous system becomes hyper-vigilant in monitoring one’s environment for threats to safety.
As data from the CDC-Kaiser Permanente Adverse Childhood Experiences (ACEs) study demonstrates, women are more likely to experience the kinds of events that lead to complex trauma and c-PTSD beginning in childhood.
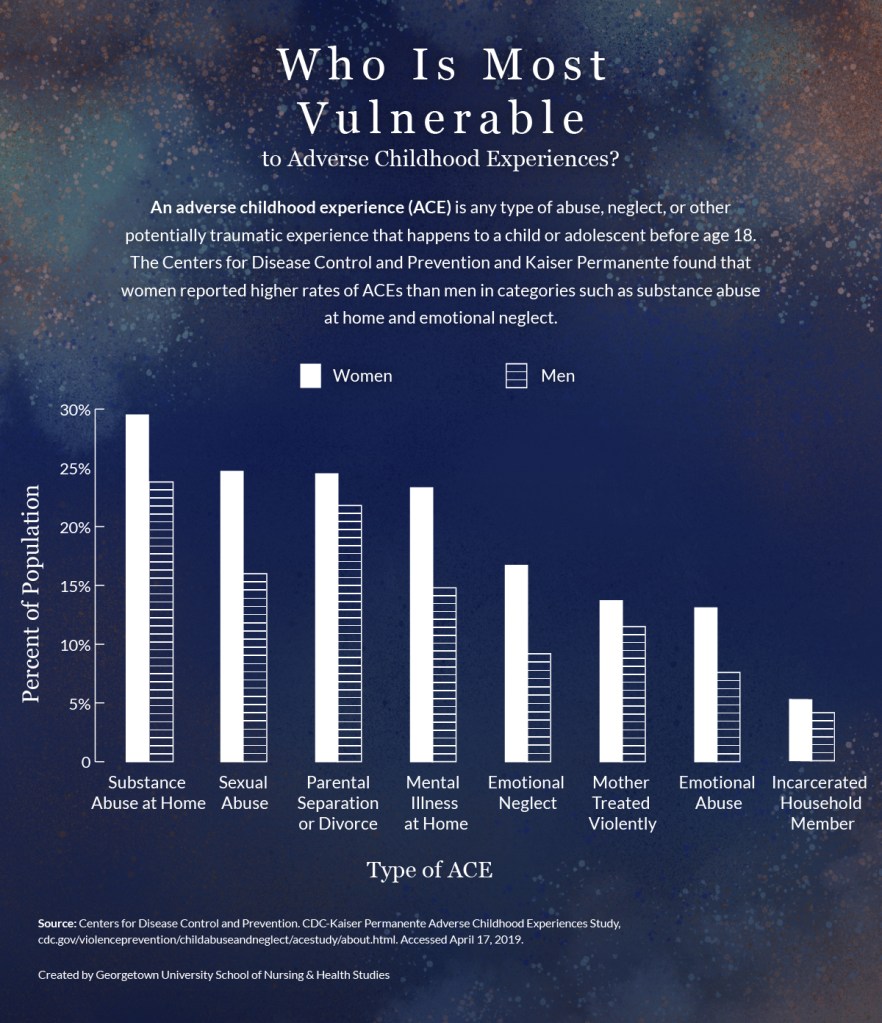
Women report higher rates than men of neglect, abuse, and adverse household circumstances experienced as children. Women are more likely to be emotionally abused (13.1%, compared to 7.6% for men), sexually abused (24.7%, compared to 16% for men), emotionally neglected (16.7%, compared to 9.2% for men), and to have a mental illness in the home (23.3% women, compared to 14.8% for men).
Go to a tabular version of Who Is Most Vulnerable to Adverse Childhood Experiences?
Women of color may be even more at risk of experiencing complex trauma and developing c-PTSD. Systemic racism creates an environment of toxic stress, said Georgetown University School of Nursing & Health Studies adjunct professor Christina Marea, MA, MSN, RN, CNM. “Toxic stress is really just the accumulation of microaggressions… combined with other types of structural bias,” Marea said.
These stressors take a toll on women’s health. Maternal health disparities in the United States demonstrate this clearly, Marea said. African American women, for instance, disproportionately experience adverse pregnancy outcomes, from pre-term birth to maternal mortality to perinatal mortality — even after controlling for the risk factors of income, education, and alcohol and tobacco use. These experiences, in turn, can become traumatic in themselves.
How Can Family and Friends Support PTSD Recovery?
Through medical attention and mental health care, women can reestablish a sense of safety. Loved ones can also play a vital role in helping women move toward health and wholeness.
Huey, a primary care provider with a background in treating depression, advocates for family-centered care, in which a woman’s health care team and family work in tandem to provide support and structure. A woman’s “family” may not be her family of origin, Huey said. Her support system might consist of a friend group or whatever she defines as family.
Mental health care, particularly related to complex trauma, is complicated. Educating a woman’s support system in addition to the patient herself is essential because stigma and lack of understanding at home will affect her condition and recovery.
“If the people who are supporting this person don’t understand what she’s going through, or what the treatment involves, it just makes it harder for that person to get better,” Huey said.
“The more support the patient has, the better outcome they will have.”
— Sally Huey, DNP, APRN, FNP-BC, Georgetown School of Nursing & Health Studies Professor
A well-educated support system can be a woman’s greatest asset in recovery from trauma and PTSD. With their knowledge of the brain and body and their experience demonstrating compassion, nurses are well-positioned to prepare a patient’s family and friends to come alongside her as she heals.
How Can Loved Ones Support a Woman Recovering From PTSD?
Counter the lingering stigma around mental health.
The nervous system reacts to stressors automatically, outside of an individual’s conscious control. One person might experience a house fire as traumatic while another may not, based on a combination of factors including childhood experiences, gender, culture, and genetics. Developing PTSD should not be considered a matter of will or weakness.
If your loved one expresses guilt about needing assistance, reframe the situation for her. Say, “If you had diabetes, you probably would not hesitate to go to the endocrinologist.” Reaffirm that mental health is no different than physical health. Both require professional care and support.
Ask how PTSD manifests in your loved one, specifically.
A symptom of PTSD is being triggered by aspects of one’s environment that bring to mind a traumatic experience. The trigger transports her back to the trauma, and she begins to feel the emotions and intense fear that she felt as the traumatic experience unfolded.
Every woman’s triggers will differ. Ask your loved one what her triggers are and how you can support her in the event that you encounter one together.
With her permission, learn more about your loved one’s care.
Offer to attend an appointment with your loved one to better understand the way PTSD affects her day to day. With her permission, set up a one-on-one phone call with her mental health provider and ask questions to better understand her condition and treatment.
Do research. Check out a book at the library, or find web sites (preferably .org or .edu) for professional perspectives.
Create an environment of safety.
Remember that your loved one is learning to re-establish a sense of safety in the world. Ask what would help her feel safe in different environments. She might need a companion to walk to class with or someone to go to the grocery store with. She may need a support person in the health care provider’s office.
Respond with compassion in the moment. Even if you are curious about the story behind the request, try not to press her for more detail than she has already shared. Remember that your role is support person, not therapist or investigator.
Break the cycle of childhood abuse and neglect.
According to counseling psychologist and trauma specialist Nancy Hensler, PhD, the single most effective intervention to prevent PTSD is addressing abuse and neglect of girls in our own families, schools, religious and governmental institutions, and corporations.
Signs of abuse can be physical or behavioral. Someone experiencing abuse may have bruises, welts, or burns that she cannot explain. She may withdraw from friends, seem afraid of her parents, or have trouble concentrating.
A girl who is neglected may be frequently absent from school, steal food or money, have trouble learning, or lack appropriate winter clothing. For more information on possible signs, refer to the sources on child abuse listed below.
If you suspect a child in your care is being neglected or abused — physically, emotionally, or psychologically — call the National Child Abuse Hotline at (800)-422-4453.
Source: Massachusetts’ Government’s Warning Signs of Child Abuse and Neglect
Please note that this post is for informational purposes only. Individuals should consult their health care professionals before following any of the information provided. Nursing@Georgetown does not endorse any organizations or web sites contained in this post.
The following section contains tabular data from the graphics in this post.
Who Is Most Vulnerable to Adverse Childhood Experiences?
| ACE | Percent of Women | Percent of Men |
|---|---|---|
Emotional Abuse | 13.10 | 7.60 |
Emotional Neglect | 16.70 | 9.20 |
Incarcerated Household Member | 5.20 | 4.10 |
Mental Illness at Home | 23.30 | 14.80 |
Mother Treated Violently | 13.70 | 11.50 |
Parental Separation or Divorce | 24.50 | 21.80 |
Sexual Abuse | 24.70 | 16.00 |
Substance Abuse at Home | 29.50 | 23.80 |
Citation for this content: Nursing@Georgetown, the online Women’s Health Nurse Practitioner program from the Georgetown University School of Nursing & Health Studies


